By Mark Thomas
Infectious diseases expert Mark Thomas explores some of the options open to New Zealand.
New Zealand is in the very early stages of an epidemic of COVID-19 disease, caused by a novel coronavirus, SARS-CoV-2. Infection with this respiratory virus causes no or minimal illness in approximately 50% of infected people, mild to moderately severe illness in approximately 48%, and potentially fatal disease in approximately 2%. Because this virus differs so much from other viruses, everyone who has not already been infected and recovered is susceptible. However, the spread of the disease through the community will result in the development of immunity in those who have been infected and survived. Once approximately 80-90% of the population have been infected, herd immunity will dramatically slow the spread of the infection in the community. (1,2)
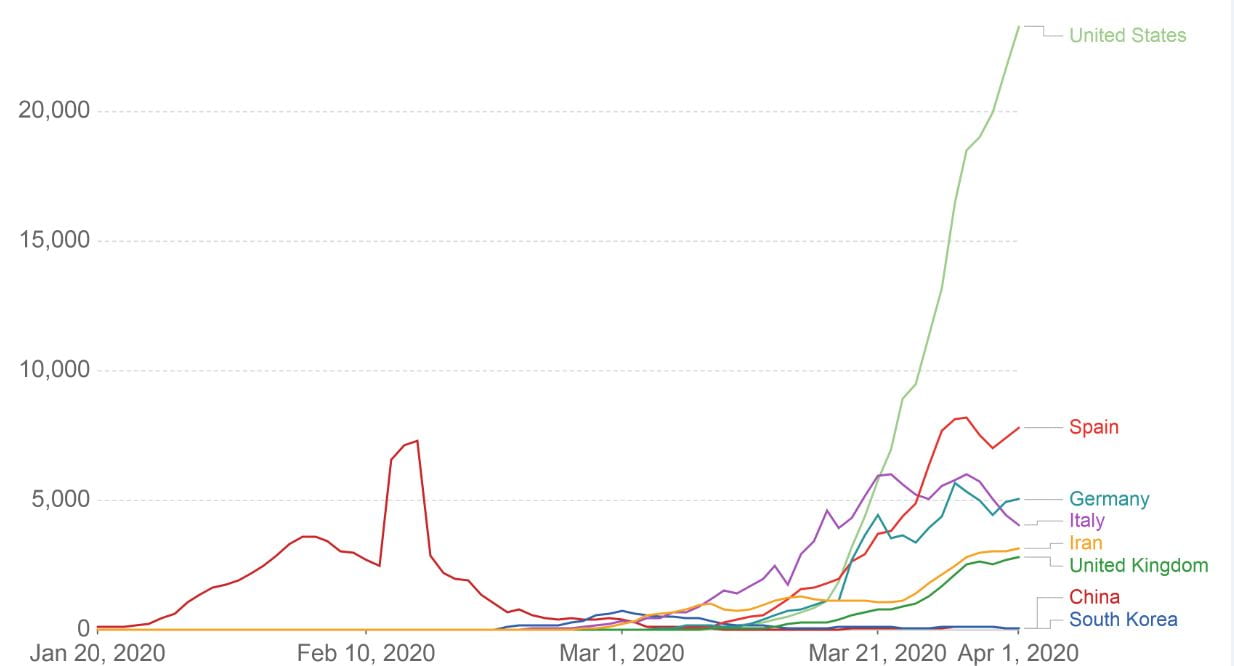
The effect of physical distancing is to reduce the reproductive number (R) – the average number of people who acquire infection from one infected person. For SARS-CoV-2, the reproductive number in most societies, in the absence of any physical distancing interventions, appears to be between two and three. Experience in China, and in many other countries, shows that strong physical distancing interventions can consistently reduce the reproductive number to less than 1, so that on average each infected person transmits infection to less than one person, and the epidemic declines, and may even temporarily cease, as shown in China. (Figure 1)
Figure 1. The number of daily new confirmed cases for several countries, between 20 January and 1 April 2020.
For all countries, to varying degrees depending on the national rates of laboratory testing, the number of confirmed cases will be substantially less than the total number of cases. The large increase in reported cases in China during 11-15 February was the result of a change in reporting methodology and did not reflect changes in actual disease incidence. Note the levelling off and/or decline in the incidence of new cases in China in February, and in some other nations in March, following the widespread introduction of physical distancing. (Reference 3)
However, if the physical distancing is relaxed prior to 80% of the population developing immunity (either as the result of natural infection or as the result of vaccination) the epidemic will inevitably recur. Because an effective vaccine is not expected to be available until late 2021, an option considered by many nations, including New Zealand, is to allow controlled spread of infection through the community. This will lead to a gradual increase in the proportion of the population who are immune. Allowing limited spread of infection through the community will inevitably result in some patients developing severe disease, but careful ongoing regulation of physical distancing may ensure that the number of patients with severe disease does not exceed the human and physical resources of our healthcare system, particularly the capabilities of hospital intensive care units.
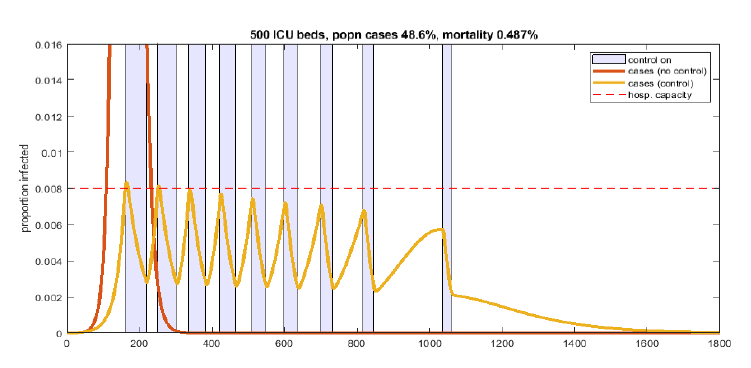
A possible strategy to allow continued spread of infection in the community, while consistently avoiding excessive numbers of severely unwell patients within the healthcare system, is illustrated in Figure 2. This strategy relies on periods of strong physical distancing interrupted by periods of less strong physical distancing. During the periods of less strong physical distancing the incidence of infection and disease will rise, while during the periods of strong physical distancing the incidence of infection and disease will fall. The duration of these alternating periods, and the strength of the physical distancing hopefully can be adjusted to ensure that the number of patients who require intensive care does not exceed the capability of the healthcare system to provide that care.
Figure 2. The effect of periods of strong physical distancing (R=0.75) shown in blue, alternating with periods of less strong physical distancing (R=1.75) shown in white, on the predicted number of cases of COVID-19 disease shown by the orange line, for a period of 1,800 days from the onset of the epidemic in New Zealand in early 2020. The solid red line shows the predicted number of cases in the absence of any interventions to slow transmission of disease in the community. The peak prevalence of symptomatic disease, in the absence of any interventions, is predicted to be approximately one person in six. The horizontal dashed pink line represents 4,000 current infections (a prevalence of approximately eight infections per 1,000 population) and approximates the infection prevalence that might result in 500 people requiring intensive care (the anticipated limit of ICU care for New Zealand in the coming year). (Reference 2)
An alternative strategy is to try to consistently suppress the transmission of infection within New Zealand, by imposing very strong border controls, a period of strict isolation for all people arriving in New Zealand, intensive case finding and isolation of any new cases, and testing and isolation of their close contacts. Because this strategy would prevent widespread transmission of infection the overwhelming majority of the population would remain susceptible to infection and disease. Therefore, this strategy would need to be maintained until after an effective vaccine had been administered to approximately 80-90% of the New Zealand population. If successful this strategy would be expected to result in much less severe pressure on hospitals, and very few deaths from COVID-19, but would require sustained, intensive, public health activity to consistently prevent transmission of infection within New Zealand, and access, within a reasonable period of time, to an effective vaccine.
References:
- Ferguson NM, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. (16/3/2020) At: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&ved=2ahUKEwjuyPONtcjoAhXt4jgGHbxWDDAQFjABegQIBRAB&url=https%3A%2F%2Fwww.imperial.ac.uk%2Fmedia%2Fimperial-college%2Fmedicine%2Fsph%2Fide%2Fgida-fellowships%2FImperial-College-COVID19-NPI-modelling-16-03-2020.pdf&usg=AOvVaw1hsNx-bJFA4q9qC2xTRHVd (accessed 2/4/2020)
- James A, et al. Suppression and mitigation strategies for control of COVID-19 in New Zealand. (25/03/2020) At: https://www.tepunahamatatini.ac.nz/files/2017/01/Supression-and-Mitigation-Strategies-New-Zealand-TPM-1.pdf (accessed 30/3/2020)
- Roser M, et al. Coronavirus Disease (COVID-19) – statistics and research. Our World in Data. At: https://ourworldindata.org/coronavirus (accessed 2/4/2020)
For more information on COVID-19, head to the Ministry of Health website.
Mark Thomas is an Associate Professor in Molecular Medicine and Pathology at the University of Auckland. He is an expert in infectious diseases.
Disclaimer: The ideas expressed in this article reflect the author’s views and not necessarily the views of The Big Q.
You might also like: